
  |
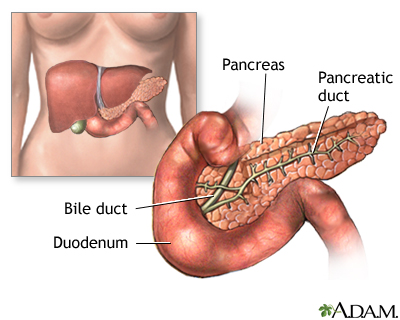
About 2% to 5% of all pregnant women will develop gestational diabetes, a type of diabetes that usually occurs only during pregnancy. With all types of diabetes, the body is unable to properly use glucose, a simple sugar that the body converts to energy. Glucose gets used by all the different cells in the body with the help of the hormone insulin, which is produced by the pancreas.
With gestational diabetes, pregnancy hormones block insulin's ability to do its job. When this happens, glucose builds up in the pregnant woman's blood.
Left unchecked, gestational diabetes can harm both the mother and the fetus. Gestational diabetes can increase the risk of:
The good news is that women with gestational diabetes can control their blood glucose levels and greatly minimize the risks.
Gestational diabetes usually starts halfway through the pregnancy. Expect to be screened for the disorder between the 24th and 28th week. You are at a greater risk for gestational diabetes than others if you:
*If you have these risk factors, you may be tested earlier than 24 weeks for the disease.
Doctors screen pregnant women for gestational diabetes by analyzing the sugar (glucose) content in a blood sample. This test usually does not require any major preparation on your part. You will drink a liquid containing glucose, and one hour later your doctor will draw a sample of your blood.
If this screening test is positive, then you will take the glucose tolerance test. You will need to fast for eight hours prior to the test. Your blood will be drawn at one, two, and three hours after drinking a sweet, glucose-rich liquid that tastes like flat cola.
The key to managing gestational diabetes is diet and exercise. Your doctor and dietitian will design a diet just for you, based on your calorie needs, weight, stage of pregnancy, and baby's growth rate. In general, the diet will be low in fat and protein and high in complex carbohydrates (bread, cereal, pasta, rice) and fruits and vegetables. You will be advised to eat three meals and one or more snacks each day. Expect this diet to change periodically to meet the fluctuating nutritional needs associated with your pregnancy and glucose control.
Your doctor may also design a safe, effective exercise plan, based on your current activity level and health. Exercises that use your upper-body muscles, but put little stress on the main part of your body, will be recommended. Upper-body cardiovascular exercise can positively effect your glucose levels. Often your glucose levels will decrease within four to six weeks of starting an exercise program.
You can see how well you are doing by testing your glucose level several times a day. There are easy ways to test your blood sugar at home. One way involves pricking your finger and putting a drop of your blood on a special strip that turns color. You cross-check the color against a color key to determine your blood sugar level. You can also buy a machine that will give you a more precise reading. If you need additional help managing your blood glucose level during pregnancy, your doctor may prescribe insulin. About 10% to 15% of women with gestational diabetes need regular insulin injections.
Your health-care team will monitor your pregnancy very closely to make sure your fetus is healthy. You may also have non-stress tests during which an electronic fetal monitor (a machine that hears and displays your baby's heartbeat) is placed on your tummy. The monitor reveals whether your baby's heart rate is increasing in a healthy way in response to movement.
You can decrease your risk of developing gestational diabetes by exercising regularly, eating a wide variety of foods from the different food groups, and establishing a healthy weight before your pregnancy.
Q: If I've had gestational diabetes, am I more likely to develop type II diabetes later in life?
A: Women who have had gestational diabetes do have an increased risk for developing type II diabetes later in life. One study indicated that more than 50% of women who had gestational diabetes developed type II diabetes within 15 years of giving birth, while another study found less than 40% developed the disease. Therefore, it's a good idea to have regular screenings for diabetes if you've had gestational diabetes. Many doctors will recommend that you have an oral glucose tolerance test at your first postpartum visit.
Q: Will my baby be born with diabetes because I had gestational diabetes?
A: Most likely not, though he or she will have an increased risk for diabetes later in life. After the delivery, a doctor will test your baby for low blood sugar. The doctor may give your baby glucose if his blood sugar is too low.